Stereotactic Breast Biopsy
- What is Stereotactic (Mammographically Guided) Breast Biopsy?
- What are some common uses of the procedure?
- How should I prepare?
- What does the equipment look like?
- How does the procedure work?
- How is the procedure performed?
- What will I experience during and after the procedure?
- Who interprets the results and how do I get them?
- What are the benefits vs. risks?
- What are the limitations of Stereotactic Breast Biopsy?
What is Stereotactic (Mammographically Guided) Breast Biopsy?
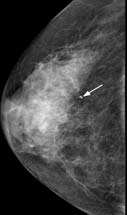
Lumps or abnormalities in the breast are often detected by physical examination, mammography, or other imaging studies. However, it is not always possible to tell from these imaging tests whether a growth is benign or cancerous.
A breast biopsy is performed to remove some cells—either surgically or through a less invasive procedure involving a hollow needle—from a suspicious area in the breast and examine them under a microscope to determine a diagnosis. Image-guided needle biopsy is not designed to remove the entire lesion, but most of a very small lesion may be removed in the process of biopsy.
Image-guided biopsy is performed by taking samples of an abnormality under some form of guidance such as ultrasound, MRI or mammographic guidance.
In stereotactic breast biopsy, a special mammography machine uses x-rays to help guide the radiologist's instruments to the site of the abnormal growth.
What are some common uses of the procedure?
A stereotactic breast biopsy is performed when a mammogram shows a breast abnormality such as:
- a suspicious solid mass
- microcalcifications, a tiny cluster of small calcium deposits
- a distortion in the structure of the breast tissue
- an area of abnormal tissue change
- a new mass or area of calcium deposits is present at a previous surgery site.
Stereotactic breast biopsy is also performed when the patient or physician strongly prefers a non-surgical method of assessing a breast abnormality.
Stereotactic guidance is used in two biopsy procedures:
- vacuum-assisted device (VAD) which uses a vacuum powered instrument to collect multiple tissue samples during one needle insertion.
- core needle (CN) which uses a large hollow needle to remove one sample of breast tissue per insertion.
How should I prepare?
You may be asked to remove some or all of your clothes and to wear a gown during the exam. You may also be asked to remove jewelry, removable dental appliances, eye glasses and any metal objects or clothing that might interfere with the x-ray images.
Women should always inform their physician if there is any possibility that they are pregnant. Some procedures using image-guidance are typically not performed during pregnancy because radiation can be harmful to the fetus.
You should not wear deodorant, powder, lotion or perfume under your arms or on your breasts on the day of the exam.
Prior to a needle biopsy, you should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to anesthesia. Your physician will advise you to stop taking aspirin or a blood thinner three days before your procedure.
Also, inform your doctor about recent illnesses or other medical conditions.
You may want to have a relative or friend accompany you and drive you home afterward. This is recommended if you have been sedated.
What does the equipment look like?
The specialized mammography machine used in this procedure is similar to the mammography unit used to produce diagnostic mammograms.
A mammography unit is a rectangular box that houses the tube in which x-rays are produced. The unit is used exclusively for x-ray exams of the breast, with special accessories that allow only the breast to be exposed to the x-rays. Attached to the unit is a device that holds and compresses the breast and positions it so images can be obtained at different angles.
At most facilities, a specially designed examination table will allow you to lie face down with your breast hanging freely through an opening in the table. The table is then raised and the biopsy procedure is performed beneath the table. At other facilities, the procedure may be performed while you sit in a chair.
One of two instruments will be used:
- A vacuum-assisted device (VAD), a vacuum powered instrument that uses pressure to pull tissue into the needle.
- A core needle, also called an automatic, spring-loaded needle, which consists of an inner needle connected to a trough, or shallow receptacle, covered by a sheath and attached to a spring-loaded mechanism.
Other sterile equipment involved in this procedure includes syringes, sponges, forceps, scalpels and a specimen cup or microscope slide.
How does the procedure work?
Mammography is a low-dose x-ray system designed to examine breasts.
The special mammography unit used to perform a stereotactic breast biopsy is a digital mammography machine. In digital mammography, as in digital photography, film is replaced by electronic detectors. These convert x-rays into electrical signals, which are used to produce images of the breast that can be immediately seen on a computer screen.
Stereotactic mammography pinpoints the exact location of a breast mass by using a computer and x-rays taken from two different angles. Using these computer coordinates, the radiologist inserts the needle through the skin, advances it into the lesion and removes tissue samples.
How is the procedure performed?
Image-guided, minimally invasive procedures such as stereotactic breast biopsy are most often performed by a specially trained radiologist.
Breast biopsies are usually done on an outpatient basis.
In most cases, you will lie face down on a moveable exam table and the affected breast or breasts will be positioned into openings in the table.
The table is then raised and the procedure is then performed beneath it. If the machine is an upright system, you may be seated next to the stereotactic mammography unit.
The breast is compressed and held in position throughout the procedure.
Several stereotactic x-ray images are taken.
A local anesthetic will be injected into the breast to numb it.
A very small nick is made in the skin at the site where the biopsy needle is to be inserted.
The radiologist then inserts the needle and advances it to the location of the abnormality using the x-ray and computer generated coordinates. X-ray images are again obtained to confirm that the needle tip is actually within the lesion.
Tissue samples are then removed using one of two methods.
- With a vacuum-assisted device (VAD), vacuum pressure is used to pull tissue from the breast through the needle into the sampling chamber. Without withdrawing and reinserting the needle, it rotates positions and collects additional samples. Typically, eight to 10 samples of tissue are collected from around the lesion.
- In a core needle biopsy, the automated mechanism is activated, moving the needle forward and filling the needle trough, or shallow receptacle, with 'cores' of breast tissue. The outer sheath instantly moves forward to cut the tissue and keep it in the trough. This process is repeated three to six times.
After the sampling, the needle will be removed.
A final set of images will be taken.
A small marker may be placed at the biopsy site so that it can be located in the future if necessary.
Once the biopsy is complete, pressure will be applied to stop any bleeding and the opening in the skin is covered with a dressing. No sutures are needed.
A mammogram may be performed to confirm that the marker is in the proper position.
This procedure is usually completed within an hour.
What will I experience during and after the procedure?
You will be awake during your biopsy and should have little or no discomfort. Most women report little or no pain and no scarring on the breast.
Some women find that the major discomfort of the procedure is from lying on their stomach for the length of the procedure, which can be reduced by strategically placed cushions. Some women may also experience neck and/or back pain as the head is turned to the side when the breast is positioned for the biopsy.
When you receive the local anesthetic to numb the skin, you will feel a slight pin prick from the needle. You may feel some pressure when the biopsy needle is inserted.
The area will become numb within a short time.
You must remain still while the biopsy is performed.
As tissue samples are taken, you may hear clicks from the sampling instrument.
If you experience swelling and bruising following your biopsy, you may be instructed to take an over-the-counter pain reliever and to use a cold pack. Temporary bruising is normal.
You should contact your physician if you experience excessive swelling, bleeding, drainage, redness or heat in the breast.
If a marker is left inside the breast to mark the location of the biopsied lesion, it will cause no pain, disfigurement or harm.
You should avoid strenuous activity for 24 hours after the biopsy. After that period of time, you will usually be able to resume normal activities.
Who interprets the results and how do I get them?
A pathologist examines the removed specimen and makes a final diagnosis. Depending on the facility, the radiologist or your referring physician will share the results with you.
Follow-up examinations may be necessary, and your doctor will explain the exact reason why another exam is requested. Sometimes a follow-up exam is done because a suspicious or questionable finding needs clarification with additional views or a special imaging technique. A follow-up examination may also be necessary so that any change in a known abnormality can be monitored over time. Follow-up examinations are sometimes the best way to see if treatment is working or if an abnormality is stable over time.
What are the benefits vs. risks?
Benefits
- The procedure is less invasive than surgical biopsy, leaves little or no scarring and can be performed in less than an hour.
- Stereotactic breast biopsy is an excellent way to evaluate calcium deposits or tiny masses that are not visible on ultrasound.
- Stereotactic core needle biopsy is a simple procedure that may be performed in an outpatient imaging center.
- Compared with open surgical biopsy, the procedure is about one-third the cost.
- Generally, the procedure is not painful and the results are as accurate as when a tissue sample is removed surgically.
- No breast defect remains and, unlike surgery, stereotactic needle biopsy does not distort the breast tissue and make it difficult to read future mammograms.
- Recovery time is brief and patients can soon resume their usual activities.
- No radiation remains in a patient's body after an x-ray examination.
- X-rays usually have no side effects in the typical diagnostic range for this exam.
Risks
- There is a risk of bleeding and forming a hematoma, or a collection of blood at the biopsy site. The risk, however, appears to be less than one percent of patients.
- An occasional patient has significant discomfort, which can be readily controlled by non-prescription pain medication.
- Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
- Depending on the type of biopsy being performed or the design of the biopsy machine, a biopsy of tissue located deep within the breast carries a slight risk that the needle will pass through the chest wall, allowing air around the lung that could collapse a lung. This is a rare occurrence.
- There is always a slight chance of cancer from excessive exposure to radiation. However, the benefit of an accurate diagnosis far outweighs the risk.
- Women should always inform their physician or x-ray technologist if there is any possibility that they are pregnant. See the Safety page (www.RadiologyInfo.org/en/safety/) for more information about pregnancy and x-rays.
What are the limitations of Stereotactic Breast Biopsy?
Lesions accompanied by diffuse calcium deposits scattered throughout the breast are on occasion difficult to target by stereotactic breast biopsy. Lesions near the chest wall may be difficult to target by this method. If the mammogram shows only a vague change in tissue density but no definite mass or nodule, this method may not be successful.
Breast biopsy procedures will occasionally miss a lesion or underestimate the extent of disease present. If the diagnosis remains uncertain after a technically successful procedure, surgical biopsy will usually be necessary.
Additional Information and Resources
RadiologyInfo:
Breast Cancer Treatment
(www.RadiologyInfo.org/en/info.cfm?pg=breast-cancer-therapy)
RTAnswers.org:
Radiation Therapy for Breast Cancer
(www.rtanswers.org/treatmentinformation/cancertypes/breast/index.aspx)
Locate an ACR-accredited provider: To locate a medical imaging or radiation oncology provider in your community, you can search the ACR-accredited facilities database.
Interventional radiology: For more information on interventional radiology procedures, visit the Society of Interventional Radiology (SIR) website at www.sirweb.org.
This website does not provide costs for exams. The costs for specific medical imaging tests and treatments vary widely across geographic regions. Many—but not all—imaging procedures are covered by insurance. Discuss the fees associated with your medical imaging procedure with your doctor and/or the medical facility staff to get a better understanding of the portions covered by insurance and the possible charges that you will incur.
Web page review process: This Web page is reviewed regularly by a physician with expertise in the medical area presented and is further reviewed by committees from the American College of Radiology (ACR) and the Radiological Society of North America (RSNA), comprising physicians with expertise in several radiologic areas.
Outside links: For the convenience of our users, RadiologyInfo.org provides links to relevant websites. RadiologyInfo.org, ACR and RSNA are not responsible for the content contained on the web pages found at these links.
Images: Images are shown for illustrative purposes. Do not attempt to draw conclusions or make diagnoses by comparing these images to other medical images, particularly your own. Only qualified physicians should interpret images; the radiologist is the physician expert trained in medical imaging.
This page was reviewed on April 22, 2013